July 28, 2020
2m 29s
Share:
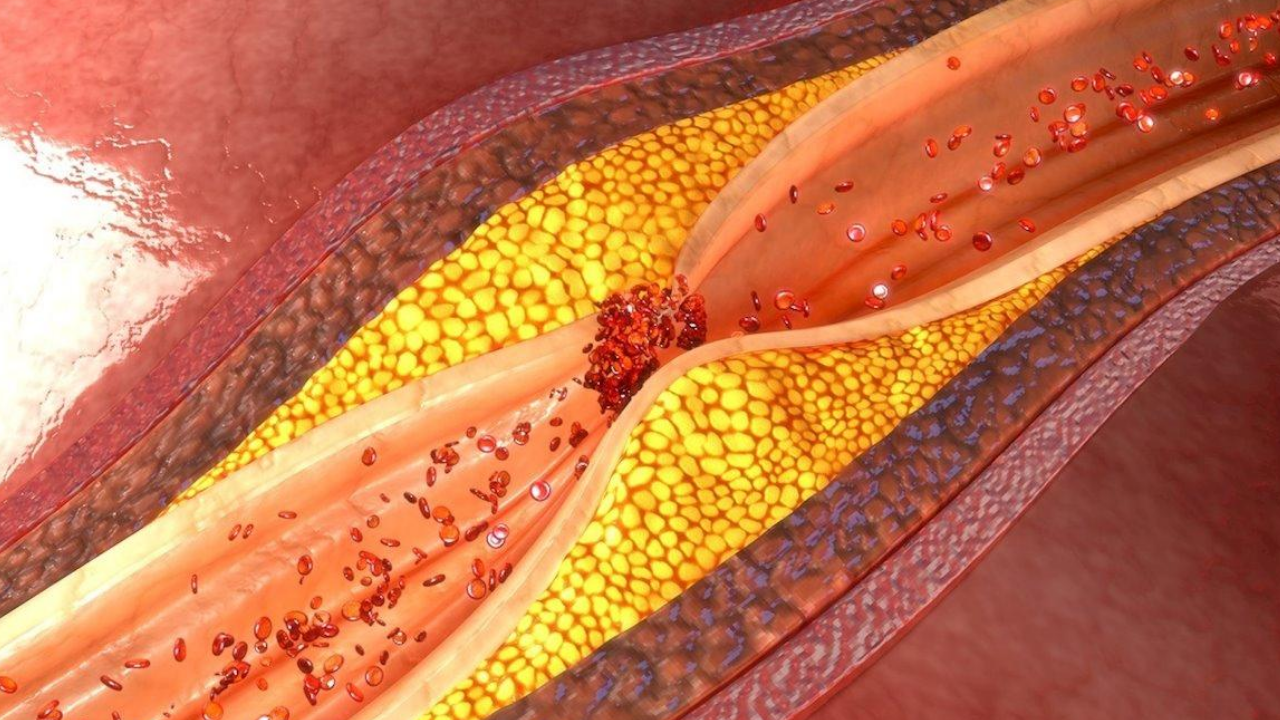
Atherosclerosis is one of the main causes of disease and premature death. Occlusive arterial pathology is one of its most important complications and has a mortality rate that can reach 60% after 10 years and 75% after 15 years. It can significantly reduce blood flow until it triggers tissue ischemia and the formation of ulcers or gangrene in the lower limbs. It is a medical, social, and economic problem that represents long periods of hospitalization, reconstructive surgeries, premature disability, etc.
Diabetes Mellitus (DM) is one of the most common diseases worldwide. It is characterized by insulin deficiency and alterations in carbohydrate, lipid, and protein metabolism. Its micro and macrovascular complications carry high treatment costs, and work disability. Diabetic angiopathy in particular accelerates the atherosclerotic process in diabetic patients and leads to a series of symptoms such as paresthesia, loss of sensations, infections, ischemic and necrotic alterations in the lower limbs.
Begic and Dilic (2019) conducted a prospective study in the Departments of Angiology, Cardiology, and Vascular Diseases of the Clinical Center of the University of Sarajevo, Bosnia, and Herzegovina. The results were published in August 2019. It was studied the progress of 80 patients divided into 2 groups of 40: one with Occlusive Arterial Pathology and injuries to the lower limbs, the other with Diabetic angiopathy, and similar injuries. All received a standardized conventional treatment that included the administration of vasodilators, antibiotics, antiplatelet agents, and statins.
Each group was divided into 2 subgroups of 20 patients: one control group and the other that received Hyperbaric Oxygen Therapy in 80-minute sessions in addition to conventional therapies. Changes in wound size and depth, granulation, exudation, and surrounding inflammation were reviewed. The statistical analysis did not show significant differences between the groups in sex, age, smoking, diagnosed HT, total cholesterol levels, LDL, or fibrinogen value at the beginning of treatment.
However, fibrinogen levels were significantly higher in patients in the control subgroups compared to those who received HBOT. The improvement in patients with Occlusive Arterial Pathology treated with HBOT was greater than in the control subgroup. In the group of patients with Diabetic angiopathy, there were no significant differences in the presence of risk factors between each subgroup, except for age or smoking, as well as a greater number of patients with HT diagnosed in the control subgroup in relation to those who received HBOT.
Furthermore, significant improvements were evident in nine patients with Diabetic angiopathy who received HBOT versus one patient who did not received Hyperbaric Treatment. This increase in the efficacy of the treatment with the addition of HBOT is related to an improvement in the prognostic of the analyzed patients. Seven of them did not receive HBOT and had a deterioration in their condition, while none of those who underwent treatment worsened.
The decrease in the diameter of the wounds and their depth, the surrounding edema, and the exudation demonstrate the properties of HBOT to enhance the bactericidal effect of antibiotic treatment, improve healing by stimulating collagen synthesis, as well as reducing stress oxidative with anti-inflammatory results and reduction of cell damage. These characteristics of the treatment make it beneficial for the diabetic population and for patients with occlusive arterial pathology, so it can be indicated after a vascular evaluation that shows non-surgical obstruction or angiopathy.
Different authors conclude that many patients with Occlusive Arterial Pathology related ulcers resistant to conventional treatment can recover with HBOT. Patients undergoing hyperbaric oxygenation mechanisms tend to normalize oxygen transport functions, reduce arterial hypoxemia, reduce HbA1c, increase myocardial contractility, decrease pulmonary hypertension, increase blood flow in the extremities, and decrease platelet adhesion and aggregation.
Source
Alden Begić, Mirza Dilić. 2019. Evaluation of the Occlusive Arterial Disease and Diabetic Angiopathy Treatment Effects by Hyperbaric Oxygenation.
Share:
Related
View cookie policy.