December 11, 2020
3m 1s
Share:
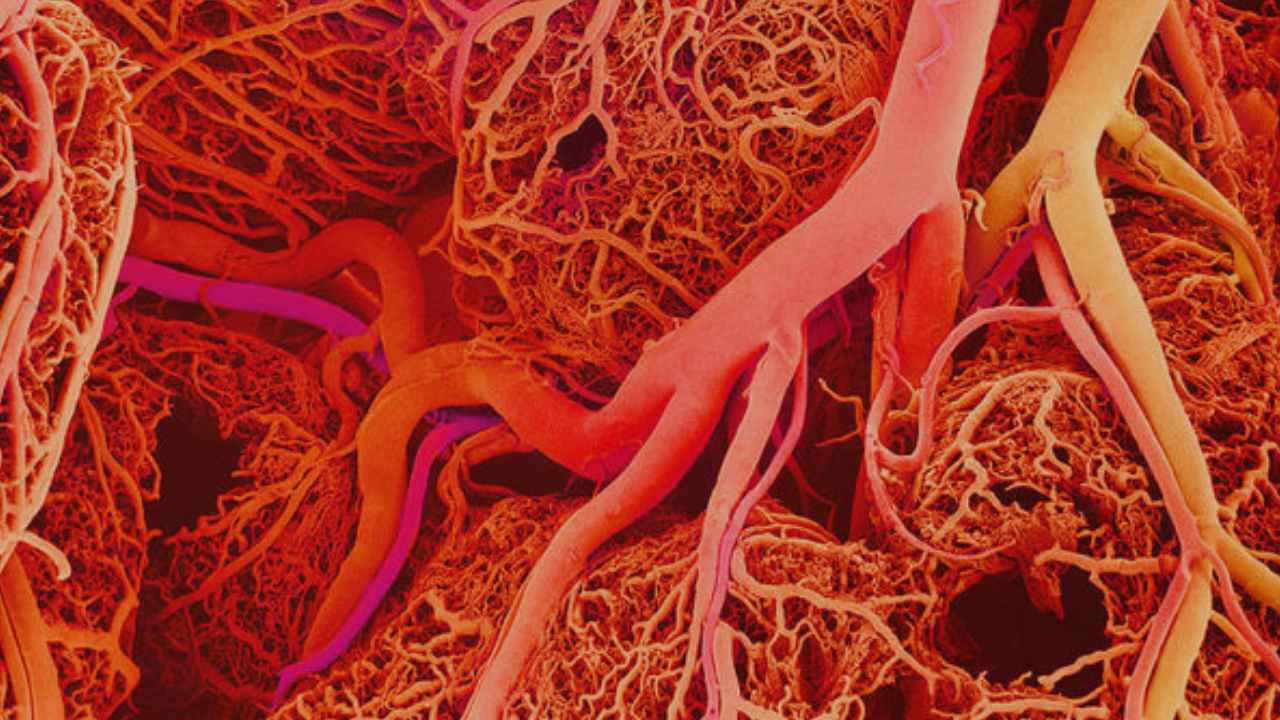
Microcirculation is a functional system that allows the adequate supply of oxygen according to the cellular metabolic demands. The microcirculation of each organ is specifically organized. In general, each nourishing artery that enters an organ branch 6 to 8 times before the arteries are small enough to be called arterioles.
The arterioles have a diameter of only 10-15 microns, they branch between two and five times and reach a diameter of 5-9 microns when they supply blood to the capillaries. They are composed of smooth muscle and, in the case of terminal arterioles, their muscular layer is not continuous.
At that point where each true capillary originates from a terminal arteriole, there is a smooth muscle fiber that surrounds the capillary and is known as the precapillary sphincter. The precapillary sphincter allows it to respond to metabolic variations.
The regulation of blood flow and the supply of oxygen and metabolites is carried out by modifying the vascular diameter. At any given time, not all capillaries supplied by a single metarteriole are perfused simultaneously. This intermittent capillary blood flow is caused by a phenomenon called vasomotion, which is due to intermittent contraction of the metarteriole and the precapillary sphincter.
The changes produced by this phenomenon contribute to a better understanding of the effect of Hyperbaric Oxygen Therapy. With high oxygen concentrations, it has been observed that vasoconstriction occurs in vessels of increasing diameters according to the degree of increase in PO2. The greatest vasoconstriction occurs in the 1st and 2nd order arterioles, while in the 3rd order arterioles there isn't any variation in the constrictive response. The greatest vasoconstriction occurred between 1 and 2 ATA with 100% O2.
Numerous studies have shown that despite a decrease in flow caused by vasoconstriction, hyperoxygenation of the arteries causes an increase in PO2 in the tissues. The uptake and transport of oxygen in ischemic areas increase with Hyperbaric Oxygen Therapy because there is an increase in oxygen concentration.
For example, Mathieu and colleagues analyzed how the hyperbaric treatment worked in 10 patients with localized ischemia and studied the transcutaneous oxygen pressure TcO2 (using transcutaneous oximetry) and blood flow (with laser Doppler flowmetry). There, they showed that cutaneous blood flow decreased in areas where oxygen pressures increased beyond normal levels, but that this decrease did not occur in areas where oxygen pressures remained below normal.
It was verified that hyperoxic vasoconstriction, in addition to preventing fluid extravasation into the extravascular space, increases tissue oxygen perfusion and favors the phenomenon of vasomotion and vascular bypass, which is the mechanism for ischemic tissue to receive blood flow in an effective way.
Another mechanism for recovering damaged microcirculation is angiogenesis and vasculogenesis, which occur as a long-term response to hypoxia. Microcirculation is repaired by increasing the production of Hypoxia Inducible Factor (HIF) and the consequent gradient of vascular endothelial growth factor and other cytokines involved in vascular repair.
The phenomenon of maintenance and recovery of the functionality of the microcirculation is not only necessary in the vascular damage of different wounds, but also prevents the development of different pathologies that involve organs such as the intestine, lung, brain, heart.
Hyperbaric oxygenation treatment also induces an increase in HIF with angiogenesis and vasculogenesis that produces repair in the vasculature of different organs where ischemia may have produced damage to the microcirculation.
In conclusion, microcirculation as a therapeutic target offers an interesting perspective for the treatment of different pathologies. Hyperbaric oxygenation produces physiological effects with a high impact on microcirculation that translate into tissue regeneration and a decrease in inflammation associated with hypoxia and recovery of ischemic organs and tissues.
Sources
Balaz, D. Komornikova, A. Sabaka, P. Leichenbergova, et al. (2016). Changes in vasomotion - effect of hyperbaric oxygen in patients with diabetes Type 2. Undersea & hyperbaric medicine: journal of the Undersea and Hyperbaric Medical Society, Inc,43, 123-134.
Sakai, T., & Hosoyamada, Y. (2013). Are the precapillary sphincters and metarterioles universal components of the microcirculation? An historical review. The journal of physiological sciences : JPS, 63(5), 319–331.
Drenjancevic, I. Gros, M. Kibel, A . (2009) Influence of hyperbaric oxygen on blood vessel reactivity: concept of changes in conducted vasomotor response. Collegium antropologicum. 33, 681-685
Donoso F, Alejandro, Arriagada S, Daniela, Cruces R, Pablo, & Díaz R, Franco. (2013). La microcirculación en el paciente crítico: Parte I: generalidades y fisiología en el paciente séptico. Revista chilena de pediatría, 84(1), 83-92
Gül, Fethi & Boran, Ömer. (2018). Microcirculation and Hyperbaric Oxygen Treatment. 0.5772/intechopen.75609.
Share:
Related
View cookie policy.