December 4, 2019
3m 50s
Share:
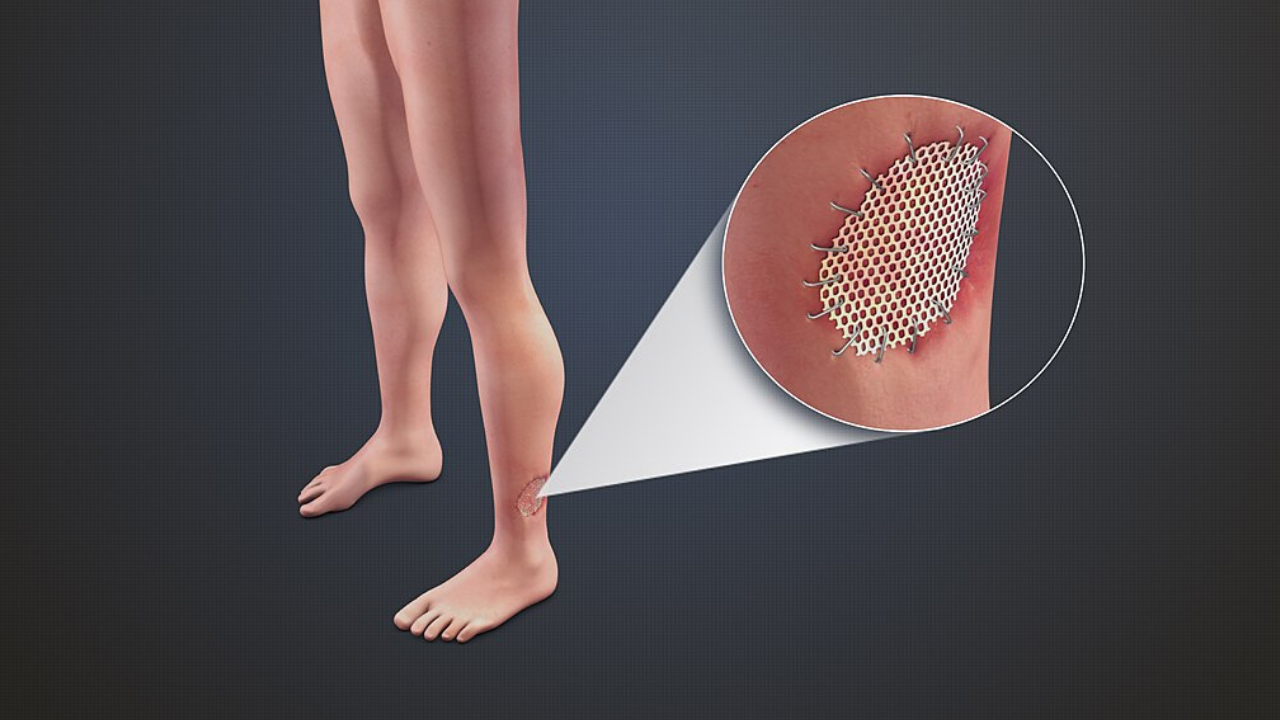
Tissue grafts and flaps are used to reconstruct wounds from trauma, chronic disease, tumor extirpation, burns, and infection. Despite careful surgical planning and execution, reconstructive failure can occur due to poor wound beds, radiation, random flap necrosis, vascular insufficiency, or ischemia-reperfusion (IR). Traumatic avulsions and amputated composite tissues—compromised tissue—may fail from crush injury and excessively large sizes. While never intended, these complications result in tissue loss, additional surgery, accrued costs, and negative psychosocial patient effects
Current treatment strategies for compromised grafts and flaps include local wound care, vacuum-assisted closure, surgical debridement, and additional reconstructive procedures. These are associated with increases in healthcare-associated costs and patient discomfort and may lead to additional donor site morbidity and negative effects on patient well-being. Hyperbaric Oxygen Therapy (HBOT) has an important and beneficial role in treating these conditions.
Hypoxia is the underlying factor in nonhealing tissue and compromised grafts and flaps, with measured oxygen tension between 5 and 20 mmHg. Oxygen is required for fibroblast function and collagen synthesis, which in turn provide normal wound healing. HBOT allows complete hemoglobin saturation with oxygen in the circulation, as well as up to 10-fold increases in dissolved oxygen plasma levels.
Plasmatic contributions to oxygenation, normally relatively minor, are increased by HBOT to levels suitable to support tissue metabolism. Given this dramatic increase, the oxygen diffusion gradient is greatly improved and favors the delivery of oxygen from the plasma to the compromised tissues. Plasmatic imbibition, the initial stage of graft healing, is therefore enhanced.
Given the success of HBOT in experimental studies for the treatment of compromised graft and flap survival, multiple studies have been undertaken to see if this effect translates to the clinical setting:
Perrins and Cantab conducted a prospective, randomized controlled clinical study that looked at the influence of HBOT on split-thickness skin grafting providing Level I evidence of the efficacy of HBOT. The authors found a 29% increased survival of the skin graft surface area. Moreover, complete skin graft take (considered >95% of surviving graft area) was noted in 64% of HBOT-treated cases compared to 17% of untreated controls.34 In addition, 100% of HBOT patients achieved greater than 60% graft take compared to 64% of controls.
Nichter et al. outlined a successful composite graft nose replantation following HBOT after near-total amputation after a dog bite.35 Given the lack of appropriate recipient vessels for microsurgical replantation and having graft dimensions exceeding the 1.5–2.0 cm limit for composite grafts, HBOT was sought as adjunctive therapy to salvage the graft. While the survival of the replanted nose cannot be attributed solely to HBOT, the authors noted a change in graft appearance from white to pink during its administration, implying a role in the graft’s survival.
Another case report documented the immediate reconstruction of a traumatic nasal defect using an auricular composite graft with adjunctive HBOT, obviating the need for a paramedian forehead flap reconstruction and its disfiguring donor site defect. It is worth noting that these and other cases of successful composite grafting are predominantly seen in the pediatric population, perhaps due to their lack of comorbidities and higher angiogenesis capability.
Bowersox et al., examined ischemic grafts or flaps in 105 patients, in which 90% had factors associated with poor graft or flap survival. In this study, *90% of compromised grafts and flaps were salvaged with HBOT.
In a retrospective study of free flaps and replantations, the authors found a positive correlation between flap/replant survival and early HBO therapy, noting 100% graft loss when HBO was started after 3 days. This clinical study again echoes the importance of prompt HBOT administration when tissue compromise is suspected. A retrospective, controlled cohort study by Roje et al. was performed on 388 patients, evaluating the effect of HBOT on short-term complications for war injury reconstructions. Skin graft loss was significantly higher in controls versus the HBOT group (52% vs. 23%, respectively). Flap necrosis was also significantly higher in the controls compared to the HBO-treated group (51% vs. 15%, respectively).
More recently, Larson et al. conducted a retrospective review of patients receiving HBOT, with 15 being treated for compromised post reconstructive flaps. Eleven patients demonstrated flap salvage: seven showed an improvement and four demonstrated complete healing. The authors noted that patient compliance and high pretreatment oxygen tension were associated with a favorable outcome. Another recent retrospective review demonstrated 75.7% successful salvage of failed flaps or skin grafts following an average of 30 HBOT sessions.
To date, the largest review of randomized controlled clinical studies on the use of HBOT on flaps and grafts was performed by Zhou et al. It encompassed 957 HBOT patients and 583 control patients and included 23 total clinical trials (16 controlled trials and 12 randomized controlled trials). The results were overwhelmingly positive with a 62.5–100% survival rate in those treated with HBOT compared to 35.0–86.5% in controls, especially if treatment was initiated within 72 h after surgery.
HBOT is not necessary for uncompromised grafts or flaps but can be an invaluable adjunct for salvage once graft or flap compromise is recognized. It is vital to promptly diagnose flap or graft compromise using clinical judgment and correct any reversible mechanical causes surgically first. If no mechanical etiology is noted or tissue compromise persists, HBOT administration should be performed expeditiously. HBOT can salvage compromised grafts and flaps, as demonstrated by numerous animal and clinical studies. In doing so, additional healthcare costs, donor site morbidity, need for multiple surgical procedures, and negative patient psychosocial effects can potentially be avoided.
Source
Ashish Francis and Richard C. Baynosa. 2017. Hyperbaric Oxygen Therapy for the Compromised Graft or Flap. Advances in wound care, volume 6, number 1.
Share:
Related
View cookie policy.