November 20, 2019
3m 48s
Share:
Skin ulcers are a dangerous and uncommon complication of vasculitis. Olivieri et al. describe the case of a teenager suffering from Systemic Lupus Erythematosus with digital ulcer resistant to conventional therapy, treated successfully with Hyperbaric Oxygen Therapy. The application of hyperbaric oxygen, which is used for the treatment of ischemic ulcers, is an effective and safe therapeutic option in patients with ischemic vasculitic ulcers in combination with immunosuppressive drugs.
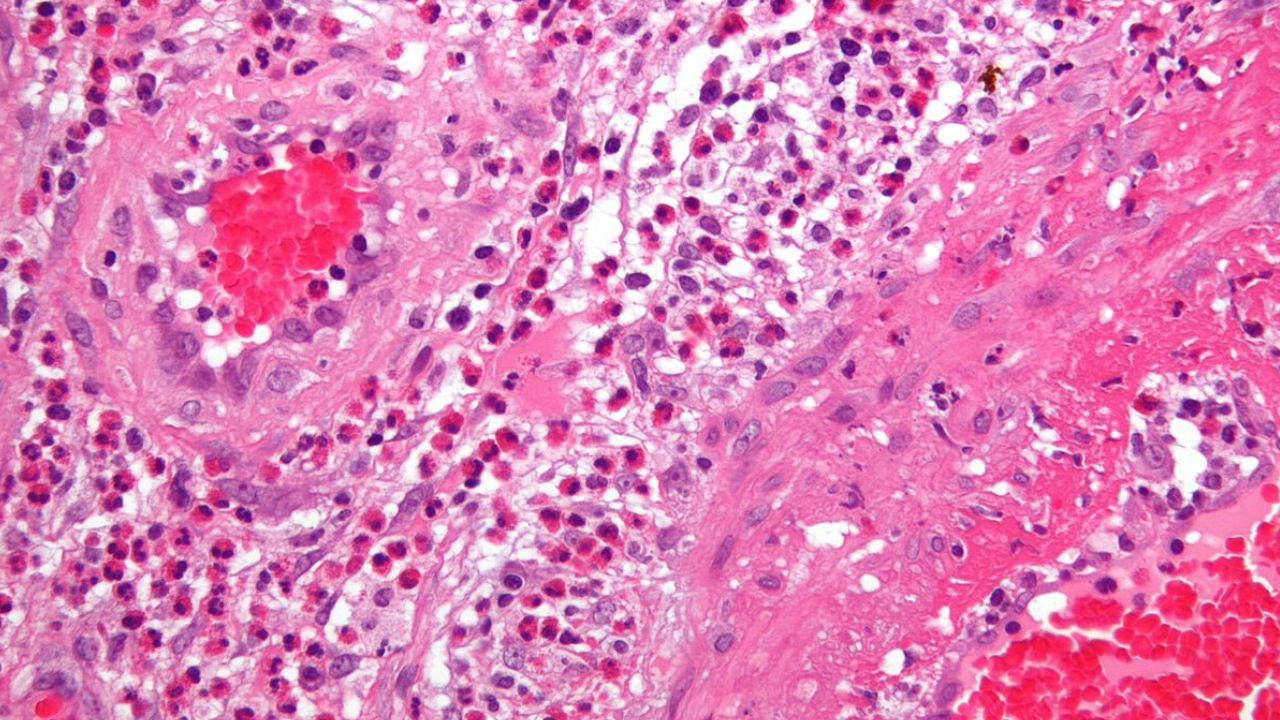
A vasculitis is a heterogeneous group of diseases characterized by inflammatory processes of the blood vessel wall resulting in the alteration of blood flow and vascular damage. The vessels involved are of different sizes (arteries, arterioles, venules, capillaries). Resulting syndromes are the consequence of tissue ischemia, vascular damage and systemic inflammation. Most vasculitis is mediated by the vascular deposition of immune complexes (IC), abnormal cell-mediated immune responses, antibodies against endothelial cells or against lysosomal enzymes of neutrophils. Vasculitis may be primary or secondary to connective tissue and intestinal diseases, medications, tumors or atopy.
Vasculitic skin ulcers are clinical manifestations of ischemic injury and are usually treated medically by controlling the underlying disease with immunosuppressants and systemic vasodilators. Hyperbaric oxygen therapy (HBOT) is used as primary or adjuvant therapy in various clinical conditions, including cutaneous vasculitic ulcers that are resistant to immunosuppressive therapy. Olivieri et al. present a case of refractory vasculitic ulcer responding to hyperbaric oxygen (HBO), which was used in combination with immunosuppressive therapy.
They decided to treat the infected ulcer of the patient with HBOT not only because it improves the oxygenation of ischemic tissues and exerts beneficial effects on vascular inflammatory response by regulating the chemotaxis of leukocytes, but also because it facilitates the healing process of infected wounds promoting the deposition of collagen, angiogenesis, epithelialization and facilitating the oxygen-dependent killing by leukocytes.
In mid-February 2008 a 14-year-old girl came under observation. She had been suffering for about 3 months from persistent fever (38 ° C), weight loss (9 kilos), headache and asthenia and was previously treated with several courses of antibiotics and prednisone. Family history shows that her paternal grandmother suffers from scleroderma, her paternal grandfather from rheumatoid arthritis, her maternal grandmother from autoimmune thrombocytopenia, and her mother from thyroiditis. At admission, she had a bodyweight of 45 kg (10th -25th percentile) and a height of 154 cm (10th -25th percentile).
Physical examination revealed a rash on the face, livedo reticularis, acrocyanosis at the first and second toe of the left foot, arthritis in knees and ankles. Blood tests showed: anemia (hemoglobin 10.5 gr/dl), leukocytopenia (3300/μl) with lymphopenia (30%), normal platelet count (289000/μl), increased inflammatory indexes (erythrocyte sedimentation rate 53 mm/1 hour; C-reactive protein 1,44 mg/dl); increased serum IgG (2270 mg/dl), lengthening of prothrombin time (57.5 seconds), reduced serum iron (16 μg/dl) and reduced levels of C3 (70 mg/dl) and C4 (9 mg/dl).
Urinalysis excluded renal involvement, and instrumental examinations (chest x-ray, abdominal ultrasound, echocardiography) ruled out the presence of serositis or other signs of disease. An eye examination, echocolordoppler of lower limbs and capillaroscopy were also negative. A diagnosis of Systemic Lupus Erythematosus (SLE) was considered and confirmed, according to the diagnostic criteria laid down by American College of Rheumatology, for the presence of antinuclear antibodies (1:1280, homogeneous appearance), anti-dsDNA (107 IU/ ml; normal < 30), anti-Sm (129 AU/ml, normal <30), antiSm/RNP (120 AU/ml, normal <30), lupus anticoagulant (1.48; normal 0-1.3) and anticardiolipin antibodies (25 U/ ml, normal up to 20).
Her lupus anticoagulant and anticardiolipin antibodies were positive on one occasion, but subsequently negative with no other evidence to suggest antiphospholipid syndrome. The patient was discharged with the following therapy: prednisone (60 mg daily); hydroxychloroquine (200 mg); anti-aggregating platelet therapy (acetylsalicylic acid); ranitidine; vitamin D3 and calcium carbonate.
After two weeks of therapy, there was an improvement in the symptoms with normalization of biochemical indices of inflammation but a worsening of peripheral cyanosis, with the appearance of an intensely painful and infected ischemic ulcer on the plantar surface of the second toe of the left foot. Echocolordoppler and capillaroscopy were again performed and were both negative. A local ulcer treatment was started with medications and cleansing performed by a consultant surgeon.
The ulcer, oval in shape, evolved in a pejorative sense at a distance of 3 months after onset, reaching a maximum diameter of about 1 centimeter. For this reason, and because of the deepening of the lesion and the risk of osteo-tendinous impairment, it was decided to associate with the medical therapy a course of HBOT, with a protocol of 5 weekly sessions of 90 minutes.
Before starting the hyperbaric therapy, the ulcer appeared painful and oval-shaped with regular margins. It was covered by an infected eschar and the surrounding skin was cold, thick and ranging from deep red to bluish in color. After a week of therapy, the cyanosis disappeared, while the ulcer healed after 16 sessions. The HBO was well tolerated by the patient and 32 sessions were carried out in total without any side effects. From the interruption of hyperbaric therapy, there were no relapses in the following months.
After four weeks from the beginning of the immunosuppressive therapy, the daily dosage of prednisone was reduced by 5 mg every 15 days; and when it reached 20 mg/day, it was further reduced by 2.5 mg every four weeks until the current dose of 10 mg/day. The immunosuppressive therapy was well tolerated by the patient, blood tests were normal and there have been no new flares of the disease.
Source
Olivieri et al. Italian Journal of Pediatrics 2010, 36:72
Share:
Related